Abstract
BACKGROUND:
Hematopoietic stem cell transplantation (HCT) is a potentially lifesaving therapy for blood cancers and other diseases. For patients without a suitable related donor, unrelated-donor registries of adult volunteers and banked umbilical cord-blood units provide potential sources of donors. Umbilical cord transplantation has several advantages including lack of adverse effects on the donor, near-immediate availability and lower risks of acute and chronic graft-versus-host disease, even with donor-recipient HLA-disparity. The main disadvantage is the low absolute number of cells in each unit, often insufficient for engraftment and timely recovery of hematopoiesis in adults. Consequently, cell dose is often the prime driver of unit selection and HLA matching criteria are much less stringent than used for adult unrelated donor HCT. Most cord blood transplantations are mismatched for one or two HLA A, B and DRB1 loci, using only intermediate resolution typing for HLA A and B. HLA C is usually not considered. However, recent data from the CIBMTR suggest that outcomes are substantially better and transplant-related mortality rates very low (~5%) when cord blood units are matched with recipients for HLA-A, B, C and DRB1 (using high resolution typing for all loci) are selected.1,2 We sought to determine the likelihood of finding a suitable 6-8 of 8 HLA-matched cord blood unit for patients in the United States, given the current available inventory, and the potential impact of technologies that would allow smaller than currently acceptable units to be used successfully.
METHODS:
Using human HLA data from the NMDP cord-blood-unit registry, we built population-based genetic models for 21 U.S. racial and ethnic groups to predict the likelihood of identifying a cord-blood unit for patients in each group. The models incorporated the degree of HLA matching and cord-blood-unit pre-freeze total nucleated cell (TNC) dose. We also calculated models that assumed that cord-blood-unit TNC dose was not a limitation.
RESULTS:
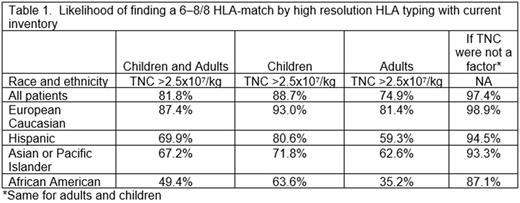
Our models indicated that currently, 81.8% of patients will identify a suitably-sized cord blood unit that is matched at high-resolution for 6-8 of 8 HLA A, B, C, DRB1 loci. This likelihood varies by patient race and ethnicity, from 49.4% to 87.4% patients as shown in Table 1. If cell dose were not an issue, these percentages increase with 97.4% of patients overall predicted to have a 6-8 of 8 HLA matched unit. Considering patient race/ethnicity, the likelihood is 98.9% for European Caucasians, 94.5% for Hispanics, 93.3% for Asian or Pacific Islanders and 87.1% for African Americans, for children and adults. The impact of TNC dose (and the potential impact of agents allowing cord blood units with smaller TNC doses to be used) is greatest for adults and people of color, particularly African Americans.
CONCLUSION:
Strategies to facilitate successful engraftment using lower cell dose units could increase the numbers of patients who could receive an optimally HLA-matched cord blood unit, with subsequent improvements in outcomes.
References:
1. Eapen M, Klein JP, Ruggeri A, et al. Impact of allele-level HLA matching on outcomes after myeloablative single unit umbilical cord blood transplantation for hematologic malignancy. Blood. 2014; 123(1): 133-40
2. Eapen M, Wang T, Veys PA, et al. Allele-level HLA matching for umbilical cord blood transplantation for non-malignant diseases in children: a retrospective analysis. Lancet Haematol. 2017; 4(7):e325-33
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.